White Paper
Understand Your Options
Sensors are transforming how medical devices function. Since most of these devices use non-disposable sensors, the design must protect the sensors from contact with medications and body fluids. This begins with selecting the right sensor for the way the device is used.
With the ever growing and aging population, patient auto-monitoring systems are becoming more and more popular. Their popularity stems from being both consistent and repeatable in addition to being low cost. Sensor-studded monitoring instruments in this category are also versatile because they can be used both in hospitals and at home. Selecting a sensor can be simple if the application and the parameters that need to be monitored are clearly understood. The most complicated sensors are implantables, followed by sensors used in catheters (through incision) and sensors used in body cavities, sensors that are external but come in contact with body fluids and sensors for external applications.
Implantable Sensors
Implantable sensors need to be small, lightweight, and compatible with body mass as well as require very little power to operate. Most importantly, they must not decay over time. Since they are Class III medical devices, they automatically require FDA approval. Implantable sensors typically require two to four years for development and implementation before moving on to production. Generally, they are more expensive and require a specialist to surgically implant them. The power requirement is one of the major challenges for implantable sensors. Sensors that can function with no power are ideal, but these are few and rare in the market. Piezoelectric polymer sensors are well suited for vibration detection since they are small, reliable, durable, and require no power. Such sensors can be used in pacemakers that monitor activities of the patient.
Temporarily inserted sensors function for a few minutes up to a few hours and require FDA approval
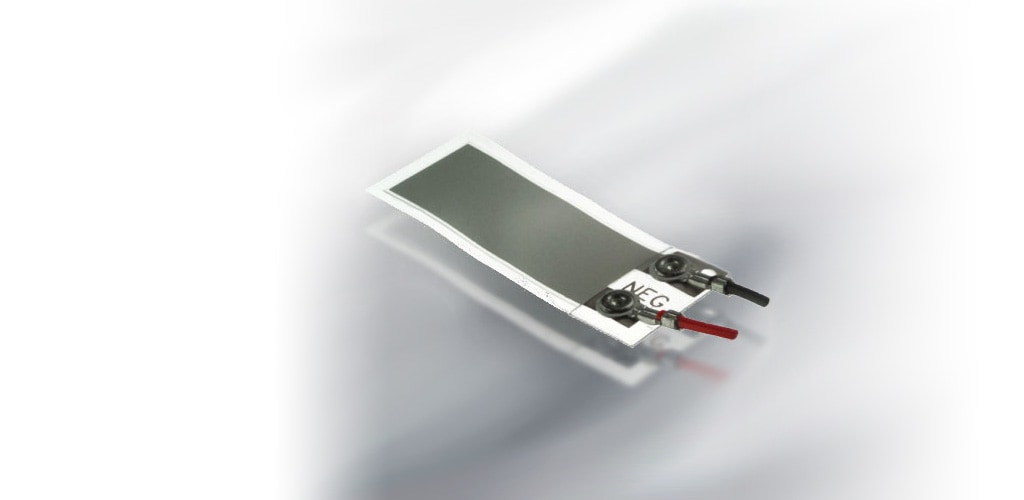
This Piezo sensor is in the shape of a tiny cantilever beam with weight attached on one end that flops with body movement. Every time the patient moves, the sensor generates a signal. Using a pacemaker as an example, the pacemaker then receives this signal and makes the heart beat at the desired pace. The sensor can differentiate between various activities such as walking, running, or other physical activities. For instance, if the patient is resting, the signal will be zero and the pacemaker will make the heart beat at a minimal rate. In this way, the sensor signal is proportional to the level of activity. A miniature Piezo film vibration sensor is 15/100 of an inch in length including the pacemaker which houses it. Implanted sensors can also be powered by external sources. For example, a Radio Frequency (RF) energy wand when placed near a sensor located inside the body will power the sensor up. The sensor will then record patient measurements, transmit the data back to the wand via RF link, and return to hibernation. Another example of using an implanted sensor in this way is that of a post abdominal aortic aneurysm procedure where an implanted sensor can monitor the pressure leaks at the surgical location.
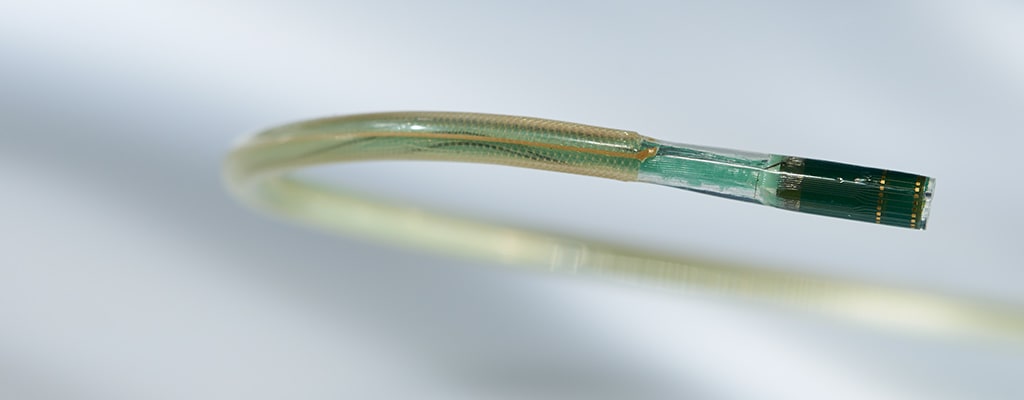
Sensors in Catheters and Body Cavities
The requirements for sensors that can be inserted through an incision – typically at the tip of a catheter – are less critical than those for implantables but will still need FDA approval. Depending on the surgical procedure, these sensors need to function for a few minutes up to a couple of hours and can be powered via external sources. A pair of matched thermistors at the tip of a catheter can be guided to different locations of the heart to measure blood flow. Either they can be heated through the coil or flushed with cold fluid to measure blood flow rates. When flushed with cold fluid, the first sensor gets cooled more than the second because the blood flow warms up the fluid that reaches the second sensor. Since these two temperature sensors are separated by a known distance where the temperature and volume of the fluid is controlled, the blood flow can be calculated by reading the difference of the resistance values of the two sensors. These thermistors do not require external power.
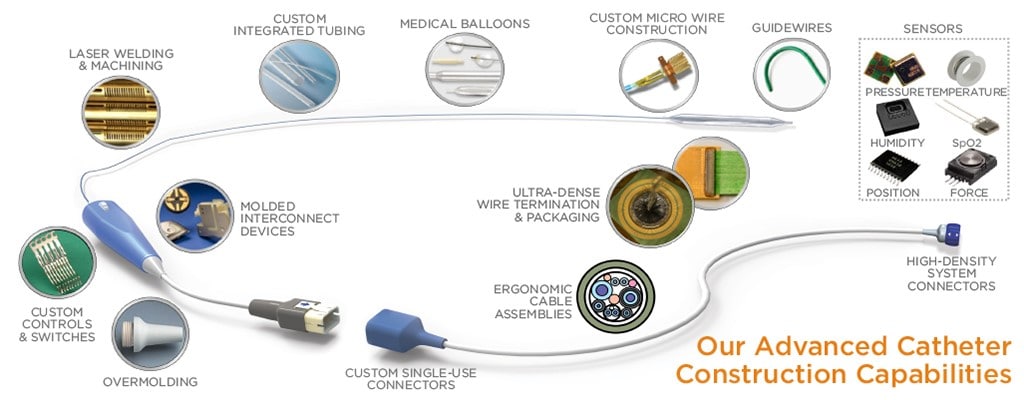
Catheter Ablation Sensors
These sensors are temporarily inserted through incision. The catheter tip contains a source for RF energy and a force load cell sensor. RF energy, like that used with implantable sensors to send data, is often used in the ablation process to burn out dead tissue. It is critical that the force applied by the catheter tip to the target tissue not exceed maximum values to avoid any possibility of perforating the target tissue. TE's sensing technology holds the promise of providing a triaxial force-sensing system able to measure tissue contact forces in all three dimensions simultaneously.
Silicon MEMS-based Disposable Pressure Sensors
These are used in intrauterine pressure (IUP) sensors to measure contraction pressure and frequency during childbirth. This method is more reliable than conventional belts and is used in critical cases. Additional features can be built into these sensors such as amnion fluid infusion and extraction. These sensors are inserted through the uterus and reside in the amniotic sac. The sensor is the taken out when the baby is ready to be delivered.
Body Cavity Sensors
These sensors include oral and rectal probes that measure body temperatures. These temperature sensors are designed to be small and rugged, and are covered with a soft coating material to protect the inner layer of the organs of the patient from sustaining damage due to contact.
Micro-Thermocouple Sensors
These sensors are flexible fine gage thermocouples used whenever fast, accurate temperature measurements are required. The thermocouple consists of two dissimilar metals, joined together at one end. A small unique voltage is produced by the two metals, which can be measured and interpreted by a thermocouple thermometer. The dissimilar metals are individually insulated, and an overcoat is present to maintain an intimate bifilar configuration (certified per ANSI MC96.1-1982). TE's Micro-Thermocouples are constructed using only bio-compatible materials, making them suitable for use in medical applications.
External Sensors Exposed to Fluids
There are several disposable sensors where the sensor is located externally from the body although body fluids come in contact with it. One example of this is the disposable blood pressure sensor (DPS). These sensors are used in surgical procedures and intensive care units (ICUs ) to continuously monitor the blood pressure of the patient. This is the reliable way to measure blood pressure when in surgery or ICU. The informational profile of the patient is then logged by plugging the disposable blood pressure sensor into a monitor. These sensors are required to be replaced every 24 hours in order to avoid contamination. Another sensor that comes in to contact with medication and body fluids is the sensor used in the inflation of angioplasty balloons. A pressure sensor at the tip of the pump will come in to contact with saline solution that is used as a media to inflate and deflate the balloon. In this application, the pressure sensor monitors the pressure applied that inflates/deflates the balloon and needs to withstand more than 200psi. If too much pressure is applied, the balloon could burst and cause severe complications for the patient.
Medical equipment manufacturers and sensor experts can create advanced technologies by working together.
TE Sensors Used in Medical Applications
- Force load cells for infusion pumps that detect occlusion (tube blockage)
- Magneto-resistive sensors in syringe pumps to detect flow rate, empty syringe and occlusion
- String pot position sensors used for remote surgical tool positioning and patient bed positioning for x-rays/CT scans
- Extremely small MEMS-based accelerometers to measure tremors in patients with Parkinson’s disease
- Piezoelectric (and also pyroelectric) sensors for sleep apnea study
- Piezo film transmitter/receiver detects presence of bubbles in infusion pumps/syringe pumps
- MEMS and load cell-based sensors for the conservation of oxygen and monitor oxygen tank levels
- NTC temperature sensors to measure skin/body temperature
- MEMS-based pressure sensors for cuff blood pressure sensor kits